Clark County emerged last year as the state leader in integrated Medicaid services. A review of the first year of integrated physical and behavioral health services shows Clark County residents are benefitting from the new approach.
Take Kate, for example.
Kate is a member of Community Health Plan of Washington — one of two health organizations providing managed care services for Medicaid beneficiaries in Clark County. Community Health Plan offered Kate’s story as an example of how the system is working locally. The organization altered the name of the member to protect her privacy.
Kate has been diagnosed with schizophrenia, congestive heart failure, hypertension and end-stage kidney failure. She’s been homeless many times over the last several years and was often hospitalized. She also frequently had conflicts with her kidney dialysis provider and would leave before completing treatment.
Neither Kate’s primary care provider nor her mental health provider knew about her issues at the dialysis center. But, after a call to the crisis line following a dispute at the center, Community Health Plan stepped in.
Kate was assigned a case manager who briefed her care providers about the issues and helped Kate develop conflict resolution skills. A community health worker accompanied Kate to dialysis appointments and helped her find affordable housing.
Today, Kate is thriving. Her mental health symptoms are improving, and she’s complying with kidney dialysis treatment. She hasn’t been hospitalized in more than nine months.
That, according to Community Health Plan of Washington, is an example of how coordinated care has been made possible under the integrated services model.
“It’s amazing to see the level of collaboration between behavioral and primary care and social support services,” said Connie Mom-Chhing, director of fully integrated managed care for Community Health Plan. “The silos have improved, from my perspective.”
Early adopter
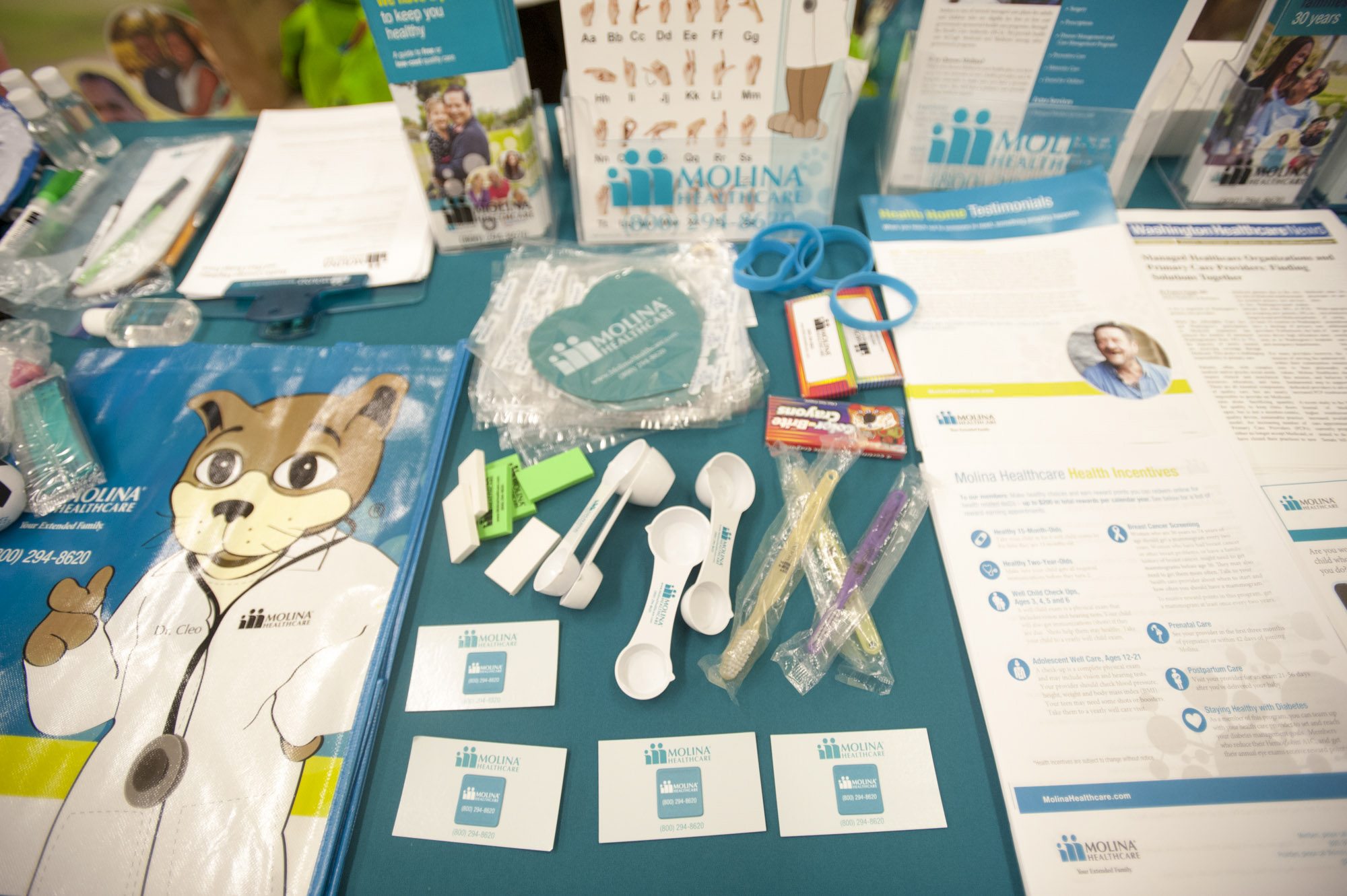
Clark and Skamania counties implemented fully integrated Medicaid managed care in April 2016. The model combines physical health, mental health and substance use disorder services under one managed care plan. In Southwest Washington, the two available plans are Molina Healthcare of Washington and Community Health Plan.
The Southwest Washington region was the first, and still the only, in the state to fully integrate the services, making it an early adopter of the model that is required statewide by Jan. 1, 2020.
Officials with the Washington State Health Care Authority, which oversees the Medicaid program, consider the adoption of integrated services in Southwest Washington a success.
“I can’t speak highly enough of the county people and the providers in Southwest Washington,” said Isabel Jones, integration policy manager at the Health Care Authority. “From the beginning, they have had such a collaborative attitude.”
The collaboration has led to improvements.
A review of outcome data from the 2016 calendar year, which includes nine months under the new model, showed statistically significant improvements in 10 outcome measures for local Medicaid beneficiaries. Eight other measures showed no statistically significant differences and one measure showed a decline. The decline was in emergency department utilization, an area in which the region was second best in the state, according to the state report.
Areas of improvement for Southwest Washington residents include adult access to preventive health services, cervical cancer screening, comprehensive diabetes care, antidepressant medication management and follow-up after an emergency department visit for alcohol or drug dependence, according to the report.
More dialogue
Community Health Plan of Washington, which manages the care for nearly 17,000 Clark County Medicaid clients, also saw improvements in additional measures.
Emergency department utilization among clients decreased 14 percent and inpatient hospitalizations decreased 30 percent, Mom-Chhing said. Community Health Plan’s clinical team is, on a daily basis, reviewing which members went to the emergency room and then coordinating with providers to establish a discharge plan, she said.
“Just because you’re successful to get them out of the emergency room, we want to make sure they’re not going back,” Mom-Chhing said.
Community health plan has also had 12 patients discharged from the Western State Hospital — something Mom-Chhing calls a “big accomplishment.” Not only are patients being discharged, but they’re being connected to a community health worker who is focused on linking the member to social support services, she said.
Molina, which manages the care for about 87,000 Medicaid beneficiaries in Clark County, is also noting improved outcomes for its members.
The number of inpatient admissions among Molina clients reduced by 15 percent and emergency department visits dropped by 17 percent, said Peter Adler, president of Molina Healthcare of Washington. In addition, of the 32 Molina clients discharged from Western State Hospital since April 2016, only two were readmitted, he said.
“That is dramatically lower,” Adler said.
The admission and readmission reductions occurred because Molina is better able to guide members to more appropriate care and to support services, Adler said.
“There’s conversation and dialogue and coordination that begins to happen,” Adler said of the integrated model. “In the past, that just didn’t happen because they were in independent worlds.”
While state officials are proud of the work accomplished in Clark County, there’s more work to do.
On Jan. 1, another region consisting of Chelan, Douglas and Grant counties will transition to fully integrated care. Five additional regions — including those with King, Pierce and Spokane counties — will make the change in 2019.
Local integration efforts will continue, too.
“It’s been a journey, and it’s not something that can be achieved overnight,” Mom-Chhing said. “It’s going to require an ongoing shaping and reshaping.”