OLYMPIA — Every time she got out of jail, Jamie Cline started hustling again for heroin, driven by an addiction she didn’t understand.
“You want to get clean so bad. You know something’s killing you and you can’t stop,” said the 33-year-old who used heroin for 10 years.
This spring was different. While in a jail work-release program, she took a medication called buprenorphine. It quieted a voice in her brain that told her to keep using.
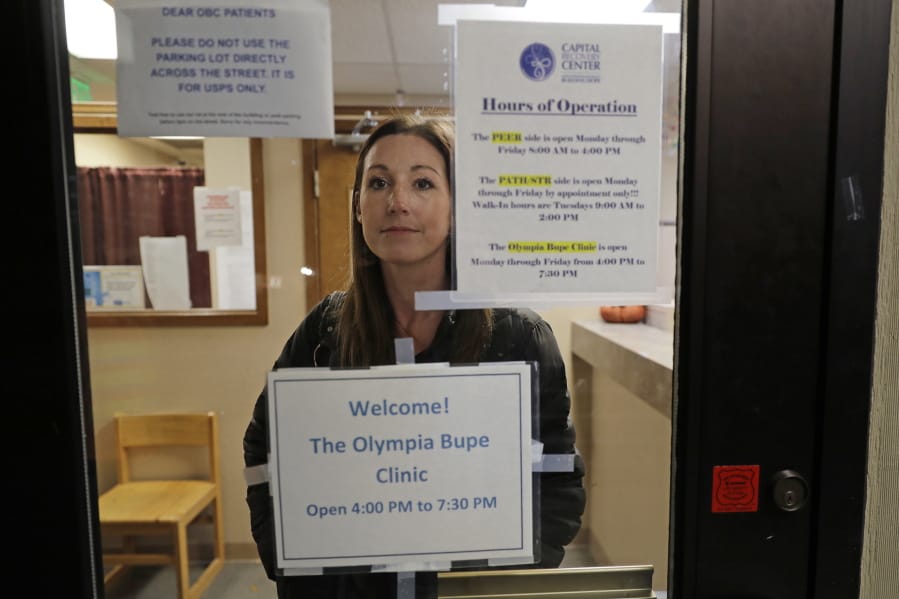
When she got out of jail, she headed for an Olympia clinic where a doctor is working to spread a philosophy called “medication first.” The surprising approach scraps requirements for counseling, abstinence or even a commitment to recovery.
Instead, it starts with fast access to prescribed medicine that prevents withdrawal sickness. After patients start feeling better, they choose their next steps.
In St. Louis, Seattle and San Francisco, people with opioid addictions can start medication on their first day of treatment. Early research suggests the approach can change lives. But it will be a tough sell elsewhere: Nearly two-thirds of U.S. treatment centers don’t offer anti-addiction drugs and there’s resistance to easy access.
Within two weeks of walking into the Olympia clinic, Cline had a job at a millwork shop. Now, nine months later, she has received a promotion and a raise, rebuilt relationships, found a room in a sober house and is proud to display a chain of “Clean & Serene” key fobs she earned from Narcotics Anonymous. She takes buprenorphine twice daily.
“I’ve got my life back,” she said.
The opioid crisis now kills more Americans than car crashes and is estimated to cost more than $500 billion a year. The epidemic is driving new treatment strategies for the 2 million Americans addicted to opioids.
Bupe, as it’s known, isn’t new. Approved to treat opioid addiction in 2002, it blocks the effect of other opioids and eases withdrawal. It’s an opioid, but an imperfect fit for the brain’s receptors, so its effect is mild and it doesn’t cause a high. It also lowers the danger of overdose and raises the likelihood a person will stay in treatment.
But finding a prescriber without a waiting list is difficult. Guidelines say bupe should be used alongside counseling, which some doctors don’t feel equipped to provide.
Success stories have convinced some experts that buprenorphine should be available in homeless camps, syringe exchanges and anywhere people use drugs.
“This is an obvious thing to do,” said University of Washington researcher Caleb Banta-Green.
Stabilizing influence or false promise?
Martyn is a 57-year-old former heroin user who goes by one name. He was living in a Seattle homeless camp known as the Jungle, running errands for drug dealers.
“Toward the end, you’re not trying to get high anymore,” he said. “You’re just trying to not be sick.”
He got his first bupe prescription at Neighborcare Health, a free downtown clinic. Once stabilized, he found a spot in a sober home with help from a caseworker.
“Now I’ve got a little room in a house I share with seven other guys.” On bupe, Martyn said, “I don’t get that high feeling. And that’s OK.”
Critics worry medication-first clinics will add to the flood of opioids on the street.
The tactic could also lead to a false understanding of addiction, said Atlanta-based counselor Samson Teklemariam, who directs training for NAADAC, the Association for Addiction Professionals.
“You’re promising the public a cure,” Teklemariam said. “There’s not a pill that you can take to alleviate symptoms of true addiction.”
In Missouri, some treatment programs had shunned buprenorphine, particularly long-term, in favor of abstinence-based counseling and support groups. Some didn’t have doctors or nurses who could prescribe it. Some believed medications were a crutch that prevented true recovery.
In 2017, with overdose deaths rising, Missouri tied federal grant money to a medication-first philosophy. Programs would get money only if they started clients on meds rapidly and if they dropped rules about medication time limits and attending counseling.
The result? Medication treatment increased and more patients stayed in treatment longer, said Rachel Winograd of University of Missouri-St. Louis who studied the implementation.
There’s pushback in Missouri from those who see the idea as at odds with “full and thriving recovery,” Winograd said. “The state is saying, we can do both.”
Research is beginning on the idea. In New York, 250 drug users will be enrolled at syringe exchanges. Some will be randomly assigned to get same-day bupe prescriptions and others will get standard care.
“If the older treatment philosophies were working, we wouldn’t have the problems we’re having today,” said Dr. Aaron Fox, who is leading the study.