CHICAGO — There’s no cure, thousands of people continue to die every week, and the economy is tanking, leaving an increasingly anxious, frustrated and fearful populace.
So goes the U.S. battle with COVID-19. That leaves people pining for a big fix, with much attention centered on one great hope: an effective, widely available vaccine that would allow them to again embrace friends, go back to work and ditch that lurking feeling of dread.
Devising a vaccine is a complex, multistep process that typically takes at least five years and sometimes a decade or more. In some cases, the efforts never succeed.
Yet scientists have great expectations this time around. They note the current worldwide focus on vaccine development, recent leaps forward in biotechnology and the federal government’s declaration of Operation Warp Speed, a multibillion-dollar taxpayer funded effort to ramp up production of vaccines even before scientists determine which one will be effective and safe.
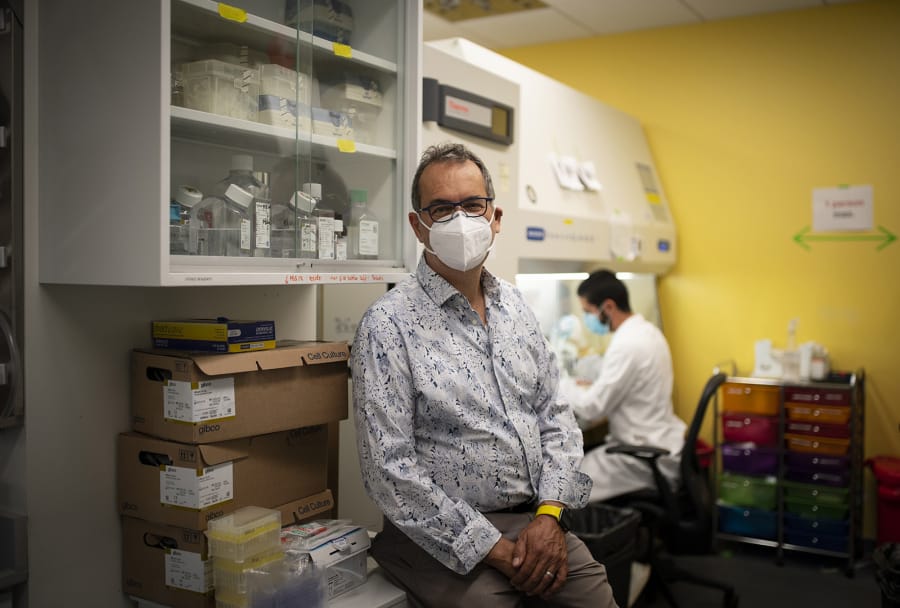
“Right now, we pray that this will work,” said Dr. Kathleen Mullane, an infectious disease expert at University of Chicago Medicine who has been involved in clinical vaccine trials. “We might be able to expect to see a vaccine available commercially either by next fall or Christmas not the coming one, but a year from now.”
Until vaccines are widely available and enough people are immunized, the usual warnings will hold: Avoid large gatherings, keep your distance, wear a mask and wash your hands.
HOW VACCINES WORK
The goal of vaccination is to prevent someone from getting infected with the targeted disease or give their immune system the tools to quickly defeat the infection if it occurs. Some do both.
The idea is to trigger a robust immune response to the attacking virus or bacterium the same type of bodily reaction that in most cases is able to defeat the infection and prevent a recurrence but without causing the life-threatening illness.
“We want the vaccine to do as well as severe disease in inducing an immune response, but not have any severity with it,” said Dr. Stanley Perlman, a University of Iowa professor of microbiology and immunology who has studied coronaviruses for 38 years.
A successful vaccine will protect most, but not all, of the individuals it’s given to. The ultimate goal is to vaccinate enough people that it becomes very hard for the disease to spread. This kind of community protection is commonly called herd immunity.
“Vaccines don’t prevent anything vaccination does,” Dr. Barry Bloom, a professor of public health at the T.H. Chan School of Public Health at Harvard University, said in a recent forum.
The vaccination percentage that is necessary to achieve herd immunity varies from disease to disease. Many scientists estimate that for COVID-19 the necessary percentage is around 60%.
But doctors and public health experts worry that not enough people will get vaccinated to reach that target, given the government’s involvement in the effort at a time when trust in institutions is waning and an anti-vaccination movement is alive and well.
“Polls show that less than half of Americans would take the vaccine,” Perlman said. “That has to change a lot.”
Indeed, a recent poll and a separate survey each found reluctance or refusal to take a vaccine in a significant portion of the population. The hesitancy is particularly great in the Black community, which has the highest rate of mortality from COVID-19.
Chicago Mayor Lori Lightfoot has taken note of the problem, saying the city will develop a vaccination education program to boost the numbers if a COVID-19 vaccine becomes available.
“I hope that people if we see that it’s effective of course will follow through and get the vaccine to protect their families, protect their friends and everybody else in the world,” Mullane said.
BUILDING A VACCINE
Many vaccines are based on a weakened, partial or killed virus or bacterium that still triggers the necessary immune response. Toxins caused by a targeted bacterium are sometimes also used.
In addition, scientists for years have been trying to use RNA, a genetic building block, to cause the body to produce a type of toxin called an antigen that would provoke an immune response. It’s hoped that such vaccines will be safer, less expensive and easier to manufacture.
Once a potential vaccine shows promise to work in a test tube, it is typically tried on small animals and then primates. If that all goes well, the research moves into the human trial stage.
Testing for safety is the focus of phase 1 trials.
“The essence of that is do no harm,” Bloom said. “No vaccine can be given to anyone if there’s a reasonable likelihood they will be harmed by it.”
The first phase can also involve scientists measuring the body’s immune response to the vaccine, to make sure they are headed in the right direction.
Phase 2 is based on a larger number of human subjects and involves identifying the proper dosage one that minimizes any side effects while still prompting an adequate immune response. Several vaccine candidates have passed that hurdle and are now in phase 3.
In that next phase, thousands of people get the vaccine and a relatively equal number receive a placebo. Then the groups’ rates of infection are compared to see if vaccinated people fare better. Ideally, the test subjects are people who are more likely to be exposed to the virus because they live in hot spots, work at jobs where exposure is more likely or are part of a racial or ethnic group in which the disease is causing more illness and death.
Often, phase 3 can take years, as scientists wait to accumulate enough data to draw final conclusions. But for COVID-19, trials are being accelerated by enrolling more test subjects from the start and then tracking them over time on a compressed schedule that Bloom called “revolutionary.”
But that tighter timeline raises some concern among scientists. A vaccine could be approved, only to have harmful effects show up months or years later, after millions of people are inoculated, they say.
And with the November election approaching, some scientists fear a rush to judgment for political advantage particularly after the Food and Drug Administration OK’d emergency use of hydroxychloroquine as a COVID-19 treatment, as well as scores of coronavirus antibody tests, only to rescind those approvals.
Bloom said there’s reason to fear “an October surprise” from the FDA where a vaccine could be rushed into emergency use without waiting for all the data from phase 3 to be collected and analyzed.
“That would really I think compromise what little trust we have in this country left about, A, vaccines in general and, B, the government’s controlling or regulating vaccines to protect the public interest,” he said.
There’s also a phase 4, which involves tracking everyone who’s been vaccinated for years after inoculation to see if any adverse effects show up later. For example, it took years to fully understand that a 1960s measles vaccine, no longer in use, could cause serious illness in some people.
PREVENT OR PROTECT?
One thing scientists conducting the trials hope to discover is whether the vaccine will prevent disease or just fight it.
If the vaccine is able to fight the disease, that would be “nothing to sneeze at,” according to Harvard epidemiology professor William Hanage. But, he said, it wouldn’t have the same broad public health advantage of a vaccine that prevents infection and leads to herd immunity.
If a vaccine does prevent infection, scientists will then ask in what percentage of the population it works.
The goal set by the federal government is at least 50%, which isn’t out of line with annual flu vaccines. But at just 50% protection, twice as many people would have to be inoculated to achieve herd immunity than would be necessary if it were 100% effective which is never the case with any vaccine.
“I think having expectations that everyone who gets a COVID vaccine will be guaranteed protection is something that is an unrealistic expectation,” Bloom said.
There’s also the question of how many shots will be needed, and how long vaccine immunity will last both of which could vary from one vaccine to another. If immunity is shorter lived, annual “boosters” could be needed.
CURRENT EFFORTS
The worldwide quest for an effective vaccine for COVID-19 has spawned more than 100 candidates, several of which have progressed to final testing just nine months after SARS-CoV-2, the novel coronavirus that causes the disease, was identified in China.
The rapid progress was made in part because Chinese scientists quickly mapped the virus’ genome and shared that information with the rest of the world.
The efforts also were aided by previous research on coronaviruses other than SARS-CoV-2 and the fact that a certain protein is widely accepted as the most crucial target for a vaccine. That so-called S protein is a spike that sticks out from the surface of the virus, allowing it to invade cells. If a vaccine can trigger production of neutralizing antibodies that block the invasion, the virus can’t infect.
Also speeding development is the U.S. government’s commitment to help cover production costs, given that vaccine-producing factories can cost more than $1 billion to build. Federal scientists also are teaming up with some private companies on the research and trial costs.
“That’s what Operation Warp Speed has been about, just getting money to these companies so that the government takes the financial risk rather than the company,” said Jeffrey Hubbell, a University of Chicago professor who specializes in bioengineering and is involved in early-stage vaccine development.
Producing vaccines on the assumption they will work is a gamble, Hubbell said. “But it’s better to place those bets than not place those bets.”
PRODUCTION AND DISTRIBUTION
Some of the phase 3 trials underway could be ready for analysis before the end of the year, but that doesn’t mean a vaccine will quickly be available to everyone.
The results must be reviewed by many scientists, then be submitted for FDA approval. If the vaccine is sanctioned, production has to be dramatically ramped up, because it will take millions of doses in the United States, and billions around the world, to get the job done.
“We have no company at the moment that could make 200 million doses for Americans or 5.6 billion doses to get 60% of the world’s people protected against coronavirus,” Bloom said. “And that explains why there has been support for multiple, different vaccines.”
If there are multiple effective vaccines, broad availability to the public could come as soon as mid-2021, Bloom said. If it’s just one or a couple, it would likely be at the end of next year.
Once the vaccines are produced, they have to be distributed. It’s a tightly controlled process and sometimes involves keeping the vaccines cold or even frozen. The mRNA vaccines, for example, would need to be stored at below-zero temperatures.
When vaccines start to become available, the government will have to determine who should get them first. One school of thought is that they should first go to people most at risk: health care workers, nursing home residents and staff, prisoners, essential workers and people in hard-hit areas. Another says vaccines should go first to groups thought to be “spreaders” perhaps college students or other young people.
Perlman, who sits on a federal advisory committee that deals with this question, said it’s possible that millions of doses could be available for health care workers and other vulnerable people before the end of the year.
THE CANDIDATES
Some vaccines in the final testing stages include:
The Oxford vaccine, being developed in conjunction with international drug firm AstraZeneca. It was made by taking a virus from chimpanzees, weakening it so it won’t harm humans and attaching DNA coding that creates the S protein in SARS-CoV-2.
Initial stages of testing found the vaccine triggered an immune response that included not only production of a neutralizing antibody that blocks the virus from invading cells but also the mobilization of the body’s T cells. These cells attack and kill infected cells, and they also can bring on a faster immune response.
“You want both, if possible,” said Mullane, the infectious disease expert at U. of C. Medicine. “You’d like to have a vaccine that will prevent uptake of the virus, but also one that activates the T cells as well to capture any virus that may have escaped the system you’ve set up to prevent infection.”
Some vaccines in the final testing stages include:
The Oxford vaccine, being developed in conjunction with international drug firm AstraZeneca. It was made by taking a virus from chimpanzees, weakening it so it won’t harm humans and attaching DNA coding that creates the S protein in SARS-CoV-2.
Initial stages of testing found the vaccine triggered an immune response that included not only production of a neutralizing antibody that blocks the virus from invading cells but also the mobilization of the body’s T cells. These cells attack and kill infected cells, and they also can bring on a faster immune response.
“You want both, if possible,” said Mullane, the infectious disease expert at U. of C. Medicine. “You’d like to have a vaccine that will prevent uptake of the virus, but also one that activates the T cells as well to capture any virus that may have escaped the system you’ve set up to prevent infection.”
A vaccine being developed by Massachusetts-based Moderna in conjunction with the National Institutes of Health. It uses what’s called messenger RNA, or mRNA, to trigger an immune response. Operation Warp Speed to date has committed nearly $2.5 billion to the Moderna effort.
The mRNA sends signals to the body to create a piece of the virus, but not the whole thing, in the hopes that the benign piece triggers an immune response. Early indications are that this vaccine too can produce neutralizing antibodies and activate T cells, and the government is moving forward with trials involving 30,000 people.
If the mRNA vaccine gets approved, it will be the first of its kind to be deployed, although experimentation with that type of vaccine has gone on for some time. “The mRNA vaccines are completely unproven, but they hold a lot of potential,” Hubbell said.
Another mRNA vaccine from the pharmaceutical company Pfizer and German company BioNTech that Pfizer says also is triggering neutralizing antibodies and T cells. Through Operation Warp Speed, the federal government has agreed to pay $1.95 billion to mass produce the Pfizer and BioNTech vaccine if it proves safe and effective.
A more traditional vaccine from Sinovac, a Beijing-based company, which has launched a phase 3 trial in Brazil. The vaccine uses an inactivated human virus to trigger an immune response. That method, however, has the potential to actually make an infection worse in a little understood reaction that sometimes occurs with such vaccines.
A deactivated human virus vaccine approved Aug. 11 by the Russian government even before it underwent phase 3 testing. Scientists expressed concern that this vaccine could turn out to be harmful later.