Nearly 3,000 people have died of COVID-19 in Washington and upward of 1,100 are hospitalized now with the disease.
A fall wave of infections has shuttered bars, glued children to computer screens rather than whiteboards and forced hospitals to delay life-altering surgeries.
Experts promised a dark winter. Hold on for vaccines, they said: The cavalry is coming.
Now it’s here.
With the Food and Drug Administration’s first emergency approval Friday night of a coronavirus vaccine, the country faces a herculean task — vaccinating most of the United States’ 330 million residents.
“The magnitude is unprecedented,” said Andy Stergachis, professor of pharmacy and public health at the University of Washington.
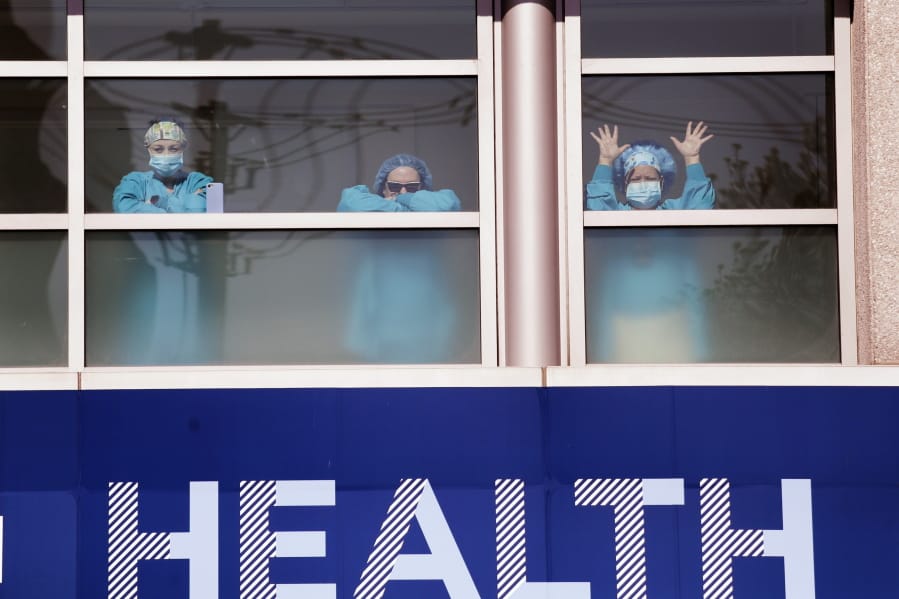
The federal government shoveled billions of dollars into developing and distributing coronavirus vaccines. Early success hinges on historically underfunded public-health agencies in the midst of a 10-month crisis, and also hospitals, whose tired employees are scrambling to head off a surge of disease and death. Now they must immunize themselves so they can protect others against the disease.
Doses of vaccine could begin arriving at hospitals early this week.
“This is PPE in the ultimate form,” said Gordon Oakes, director of clinical support services at Bellevue’s Overlake Medical Center, comparing the vaccine with the gloves and masks that protect against infection.
The FDA agreed the Pfizer vaccine was 95% effective after a second dose in a clinical trial that involved nearly 44,000 people, according to an article in the New England Journal of Medicine.
Between the Pfizer vaccine, and a similar product from Moderna that awaits emergency approval, state officials expect more than 400,000 doses from the federal government by the end of 2020, which will go to hospitals for health care workers and residents in long-term care facilities.
State officials Thursday further refined which health care workers should get the first doses, asking hospitals to use “clinical judgment” to direct the vaccine to those with the highest risk, including people who treat patients face-to-face, testing-site staffers and first responders with the most risk of exposure.
Hospitals gear up for vaccination push
With a record number of patients receiving treatment for COVID-19 in hospitals, protection comes none too soon for hospital workers.
Several King County hospitals, including UW Medicine and Swedish, are among the first 17 sites to receive vaccine and plan to begin vaccinating next week. Other hospitals, such as Overlake and Evergreen, will receive shipments a few days later and plan to begin vaccinating the week of Dec. 21.
But protecting staffers, and ensuring they can continue to care for patients filling hospital beds, will require delicate scheduling and care.
“The real manpower is not the person holding the needle,” but those registering employees, gathering consent forms and scheduling vaccinations, said Dr. Francis Riedo, Medical Director of Infectious Disease at EvergreenHealth in Kirkland.
Clinical-trial data suggests the Pfizer vaccine provides some protection after its first dose and works well across different ages, races, ethnicities, body types and preexisting medical conditions. Few serious health events were reported during the clinical trial. But for some, the vaccine will cause pain where injected, fatigue, headache, fevers and chills, among other reactions.
That could leave some staffers “feeling a little crummy,” said Dr. Shireesha Dhanireddy, an infectious-disease clinician at Harborview Medical Center who is helping lead vaccine-planning efforts for UW Medicine.
Hospitals plan to stagger vaccinations among units, such as intensive-care nurses, so they aren’t all out at once. Many have asked employees to sign up to be vaccinated ahead of time away from work, so they can lie low at home.
“We want to maintain our workforce,” Dhanireddy said, adding that vaccine reactions will be “clinically indistinguishable from COVID symptoms themselves.” Throughout the pandemic, hospitals have asked sick staffers to remain home.
Donna Jensen, chief nursing officer for Swedish Medical Group, said staff nurses could inject 975 people a day, if necessary, but they plan to stretch the first batch of vaccine out over four days, to reduce the number of staff who might need to stay home.
She estimates about 28% of Swedish employees will be inoculated in the first week.
If supply is available, and between upcoming holidays, complicated scheduling and other “speed bumps,” Riedo said he hoped to vaccinate Evergreen’s 3,500 health care workers within two to three weeks and then begin “follow-ups” for second doses.
The CDC will be monitoring those who are initially vaccinated for side effects. In addition to typical vaccine-monitoring databases, the federal agency is launching a smartphone-based program called V-Safe, which will check in with health workers about side effects and provide real-time data to regulators on any irregularities or safety concerns. The program also will remind workers to get second doses.
Beyond scheduling their own staffers, hospitals must coordinate how to vaccinate other eligible workers. Oakes said Overlake will reserve “open blocks” for high-risk first responders and is coordinating with local agencies.
The vaccine will be valuable and sought after. Stored vaccine will be locked down and in a secure location within Evergreen’s facility, Riedo said.
Jensen, of Swedish, said the medical group was beefing up security, “planning for the event that maybe there’s somebody who wants vaccine and demands it, but they’re not in the category that should get it right now. You want to be able to manage those situations.”
Swedish staff have dealt with volatile situations before during the pandemic, especially when testing was limited and people were frightened and angry. “When your emotions are involved, you can become very excitable very quickly,” Jensen said.
Questions remain on whether some hospital workers should be vaccinated. The initial clinical trial did not examine the vaccine in certain groups, including pregnant women.
“We will offer the vaccine to pregnant and breastfeeding women, with the caveat that there are no data in that group and they can discuss the risk and benefits of the vaccine with their health care providers,” Dhanireddy said Wednesday.
Unfortunately, getting vaccinated won’t allow medical workers to shed their protective gear, Jensen said. While the vaccine may be 95% effective, that means it may not work in 5% of people — and there’s no way to tell who’s protected and who’s not.
It’s also not clear how long protection will last or if the vaccine prevents transmission of the novel coronavirus.
Hospital leaders said they have strongly encouraged employees to vaccinate.
“Vulnerable people are coming in. This is a way to protect not just ourselves, but our community,” Dhanireddy said. “We can set the example.”
Pfizer will ship the vaccine in insulated boxes called thermal shippers. Vaccine recipients will also receive kits containing syringes, needles, alcohol prep pads, surgical masks and vaccination-record cards. Vaccine can be stored in ultracold freezers some hospitals have, or in the insulated packaging itself. Dry ice can be added to the packages to store vaccine longer.
Each package of vaccine, which is the size of a pizza box, will contain 975 doses of vaccine. Vials of vaccine will contain five doses each. Each must thaw and be mixed with saline solution before administered. Once reconstituted, the vaccine remains stable for six hours.
Moderna’s vaccine, which uses similar technology as Pfizer and trails it in the approval process by about a week, will remain stable in the refrigerator for 30 days and can be shipped in packages as small as 100, according to state officials.
The federal government, which is directing vaccine doses based on states’ populations, has promised Washington 62,400 doses of Pfizer’s vaccine during initial shipments, according to Michele Roberts, the state Department of Health’s acting assistant secretary.
The state had determined where about half of the initial shipments should go as of Thursday, selecting 17 sites in 13 counties with ultracold freezers. Most of those doses are for health care workers, though one package of vaccine was reserved for Consonus Pharmacy, which partners with some long-term care facilities.
Crucial test of strained public-health systems
The rollout to health care workers and long-term care residents will be a crucial test of distribution and administration systems, said Stergachis, the UW pharmacy professor, who cautioned the wider public to have realistic expectations about when vaccine will be more broadly available.
“There have been overstated goals as far as how many doses are going to be available by when,” Stergachis said.
With health care workers, nursing-home residents and other high-risk people getting early priority, vaccine for the general public may not be available until spring or summer.
The next waves of vaccination, which could include some essential workers, seniors and people with significant health risks that intersect with COVID-19, will rely on less centralized infrastructure.
Without additional federal funding, health agencies that already are stretched to the breaking point say they will be hard-pressed to orchestrate the massive undertaking.
“We’re absolutely not resourced to do this work,” Michele Roberts, Washington’s acting assistant secretary of health said in a recent briefing for University of Washington staff. Existing public-health infrastructure is set up to support routine immunizations, not an effort to vaccinate the entire population, she said.
DOH has received about $8 million from the federal government for coronavirus- vaccine work, but it will need at least $20 million more to do the job effectively and without derailing other public-health programs, Roberts estimated.
Public Health — Seattle & King County needs at least 30 additional staff for a successful vaccine rollout, at an estimated cost of about $ 4 million, immunization manager Libby Page said.
That estimate does not include the cost of supplies for vaccination clinics. Dr. Jeff Duchin, health officer for Public Health — Seattle & King County, said those clinics will be needed to vaccinate hard-to-reach populations and ensure equity.
“We are awaiting stimulus dollars,” Duchin said.
Eventually, when vaccine is more widely available, people should be able to get it at a wide variety of sites, including clinics, pharmacies and government-sponsored venues like community centers and drive-up systems, Stergachis added.
Ten months ago, EvergreenHealth’s Riedo saw some of the first U.S. patients with COVID-19 and identified the nation’s first known outbreak. Riedo helped trace transmission back to the Life Care Center, a skilled nursing facility that was sending patients to the hospital. Within a four-week-span, dozens of the facilities residents would die.
Riedo is charged now with vaccinating EvergreenHealth employees, his co-workers.
A vaccine was not a consolation to the millions around the world who have suffered or died after contracting the virus, Riedo said, but said he felt “wonder” and “gratitude” at what science had accomplished.
“We have a vaccine that’s 95% effective. It’s truly breathtaking, the speed with which this has happened,” Riedo said, adding that now the challenge was to convince everybody to take the vaccine, to protect themselves and protect those around them. “We have so much more work to do.”