Gregory Ginsberg, a Penn Medicine doctor, is exploring a new frontier in the treatment of Type 2 diabetes.
He’s co-leading a clinical trial at Penn that is testing whether killing cells on the inner surface of the duodenum — the first part of the small intestine immediately past the stomach — can lead to better control of blood sugar in people with diabetes.
Preliminary work done in South America and Europe has found that the outpatient, endoscopic procedure called duodenal mucosal resurfacing reduced A1C, a long-term measure of blood sugar; reduced the need for insulin; and reduced liver fat in people with nonalcoholic fatty liver disease. While not a cure, the procedure could allow patients with diabetes to take fewer drugs and is another sign, Ginsberg said, that cells in the duodenum play an important role in the body’s metabolic communication system.
Penn is now one of five U.S. institutions participating in a small pilot study of the procedure. Results are not yet available, but Ginsberg said the previous research has made him hopeful that he is studying a “transformative” procedure.
“This research is compelling because it harnesses the untapped potential of the luminal digestive tract in the management of health and disease,” Ginsberg said. “Moreover, it is provocative in its application of minimally invasive endoscopic therapy to treat a metabolic condition.”
The procedure had its genesis in observations about the impact of gastric bypass surgery, which creates a new path for partially digested food that bypasses the duodenum entirely. Obese patients who are diabetic and undergo the procedure often see big improvements in markers of diabetes even before they lose a lot of weight, Ginsberg said. That has triggered interest in whether the duodenum is involved in signaling other parts of the body about the need for insulin, a hormone involved in allowing your cells to use blood sugar for energy. It’s part of a relatively new avenue of research into the role the gut plays in metabolism.
“The gut is really a frontier in diabetes research,” said Raymond Soccio, a Penn endocrinologist who studies fatty liver disease and is not involved in the study.
In Type 2 diabetes, cells develop insulin resistance, which means they don’t respond properly to the hormone. (In the much less common Type 1, an autoimmune condition, the body stops making insulin.) Insulin resistance is an important factor in Type 2 diabetes, nonalcoholic fatty liver disease –most obese people with Type 2 have this — and polycystic ovary syndrome.
Soccio said bile acids, which are involved in the absorption of fat and fat-soluble vitamins, cycle between the duodenum and the liver. “They also seem to have important signaling and other functions in the liver related to diabetes and insulin resistance that we don’t fully understand.”
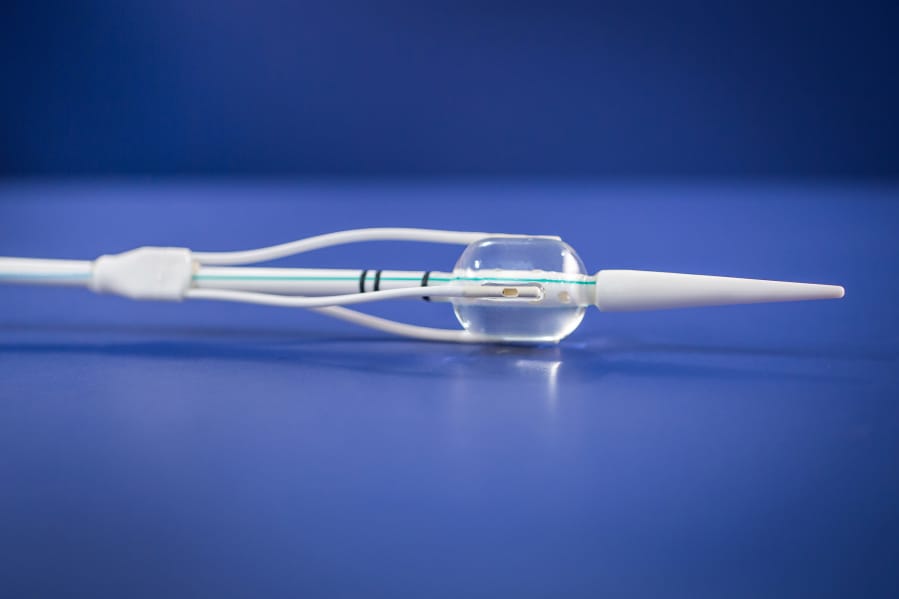
Ginsberg said that cells in the duodenum become enlarged and dysfunctional after years of exposure to unhealthy diets rich in fat and sugar. DMR uses a catheter to deliver a balloon filled with 176-degree water to the duodenum. During the procedure, Ginsberg uses the balloon to ablate or burn cells in 3/4 -inch segments over four inches of the duodenum. The hypothesis is that, when they grow back, the cells send more normal metabolic signals, Ginsberg said.
Patients in the study’s control group undergo a sham procedure that includes everything but the heated water.
The catheter was developed by Fractyl Laboratories Inc., in Lexington, Mass. Its studies abroad are looking at the impact of the procedure on diabetes, fatty liver disease and PCOS. The company has approval to begin marketing its procedure in Europe, said Harith Rajagopalan, Fractyl’s co-founder and CEO.
Results released last year from studies abroad showed the procedure is not a cure. One study found that average A1C, a measure of average blood sugar over three months, dropped from 8.5 percent to 7.5 percent after two years. Normal is less than 5.7 percent. Another small study found that 13 of 16 patients were able to stop taking insulin.