Illicit fentanyl kills at least two people every day in King County, and the powerful opioid was responsible for over 700 fatal overdoses last year, roughly triple the death toll of traffic crashes and gun violence combined.
How did the little blue pills — which were virtually nonexistent in the local drug supply just five years ago — become the most pressing public health crisis facing the greater Seattle area?
Today, The Seattle Times embarks on a collection of stories about the fast-moving fentanyl epidemic. We’ll explore how the dangerous drug has taken hold, why it’s so potent, and the ways it’s overwhelming emergency responders and the health care system. We’ll delve into how elected officials and social service providers are responding to the crisis. And we’ll explain how the opioid has disproportionately affected some of the region’s most vulnerable communities.
But first, we’ll detail how families are grappling with their grief over a loved one’s use of fentanyl, which is now a leading cause of accidental death among American adults.
Fentanyl was first introduced in the 1960s to treat severe pain, particularly for patients recovering from surgery. Some pharmaceutical-grade fentanyl made it to the streets, but at $30 to $40 a pill, it was exorbitantly expensive compared with drugs like methamphetamine and black tar heroin.
Now, however, the Mexico-based Sinaloa and Jalisco cartels, which have long run street drugs up Interstate 5, are responsible for producing the vast majority of fentanyl smuggled into the U.S.
Making the drug with precursor chemicals from China, the cartels’ chemists aren’t concerned about quality control. So the concentration of fentanyl — cut with acetaminophen when pressed into pills, and with sugars like lactose and mannitol in its powder form — varies widely from pill to pill and batch to batch.
“It is the deadliest drug threat our country has ever faced,” Anne Milgram, who heads the federal Drug Enforcement Administration, said earlier this year in testimony before the Senate Foreign Relations Committee.
More than 1,000 people died from drug overdoses in King County last year, and 70% of those deaths involved fentanyl — making 2022 the deadliest year ever for fatal overdoses countywide. Worse yet, the death toll is showing no signs of leveling off, with over 275 people succumbing to fentanyl overdoses since the start of the year.
“I’ve been waiting for a plateau … and I haven’t seen it yet. And I’m growing less optimistic I’ll see it this year,” said Bill Barbour, a death investigator with the Medical Examiner’s Office who manages the county’s real-time Fatal Overdose Surveillance Program.
EMTs, paramedics and public health workers are on the front lines of the epidemic, battling to keep people alive and introducing harm-reduction strategies that show some signs of success. Meanwhile, the Medical Examiner’s Office is not only tracking deaths but also working with other agencies statewide to identify overdose patterns and populations who face heightened risks.
“We know people who’ve had a nonfatal overdose are at higher risk for a fatal overdose,” as are people who’ve had even short periods of sobriety that cause their tolerance to wane, Barbour said. “Even with the data we’re putting out, there’s a sense we’re underreporting the scope of the problem.”
Fentanyl first hit Seattle streets in a big way in early 2019, about two years behind its mass introduction on the East Coast. By 2020, the synthetic opioid was responsible for as many King County overdose deaths as heroin, a likely consequence of the lockdowns, social upheaval and isolation brought on by the COVID-19 pandemic.
The 168 overdose deaths involving fentanyl that year more than doubled to 385 deaths in 2021, then nearly doubled again to 712 last year.
At the same time, heroin has all but disappeared from the local supply: Last year, overdoses from the county’s historically predominant street drug accounted for 92 deaths, the first time heroin was involved in fewer than 100 deaths since 2013.
Like heroin and prescription opioids, fentanyl’s danger lies in the fact that it’s powerful enough to overcome the body’s involuntary impulse to breathe.
But fentanyl is 50 times more potent than heroin, and its effects don’t last as long as other opioids, making the drug much more dangerous, said Brad Finegood, a strategic adviser on behavioral health at Public Health — Seattle & King County.
Illicit fentanyl is cheap to produce and now sells on the streets for $3 or $4 a pill, making it readily accessible. And because the high lasts only 20 minutes or so, people addicted to the drug may need 30 or more hits a day, leaving them oscillating between intense cravings and euphoria.
“The lethality risk is so high,” Finegood said. “The addiction potential is so high.”
With emergency rooms already overcrowded, fentanyl’s increasing presence in the Puget Sound area “is definitely having an impact on the entire health care system,” said Dr. Michael Sayre, the Seattle Fire Department’s medical director.
Even people who initially survive an overdose can die days later or suffer irreversible brain injuries, said Sayre, who also practices emergency medicine at Harborview Medical Center.
“There just isn’t enough access to treatment,” he said. “It needs to be accessible” whenever someone is ready to accept help, “whether that’s at 4 in the afternoon or 4 in the morning.”
Fentanyl’s potency also means people who exclusively use stimulants like cocaine and meth can easily die if the white powder they ingest turns out to be the synthetic opioid, which is increasingly being funneled into the local drug supply in unpressed powder form.
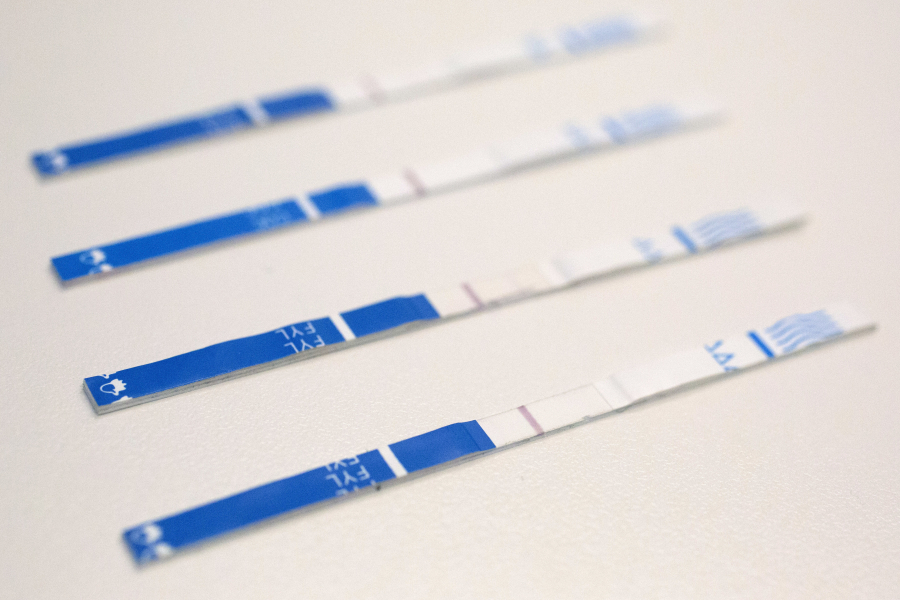
To protect against that scenario, Public Health officials in 2022 distributed 100,000 fentanyl test strips to organizations that aid people at higher risk of overdose, as well as to bars and nightclubs for use by their patrons. The department has also worked to make naloxone — a nasal spray also known by the brand name Narcan that can quickly reverse the symptoms of opioid overdoses — readily available throughout the county, distributing the drug at hospitals, clinics, needle exchange centers, vending machines and, most recently, hotels and event venues. King County residents can also order free naloxone kits online.
The increased prevalence of naloxone now means there’s a good chance a bystander has already administered the drug to an overdose victim by the time paramedics arrive. And there are signs that more people are at least attempting to reduce the risks inherent in fentanyl use: Death investigators are increasingly finding naloxone, unopened test strips or unfilled prescriptions for Suboxone, a medication used to treat opioid addiction, at fatal overdose scenes.
Sadly, however, investigators are also finding multiple bodies at some scenes, indicating people are getting the message not to use fentanyl alone but that no one in a group stayed sober long enough to make sure the others were still breathing.
“I see these families just longing for any details about their loved ones,” said Barbour, of the Medical Examiner’s Office. “Behind every single number is this wake of hurt.”
Editor’s note: A previous version of this story misstated the emphasis of Public Health — Seattle & King County’s fentanyl test strip distribution efforts. Agency officials in 2022 distributed 100,000 test strips to organizations that aid people at higher risk of overdose, as well as to bars and nightclubs for use by their patrons.