Choosing the right antidepressant can be a daunting task. With so many choices and such unpredictability in their individual effects, patients with depression often spend months or years casting about for the right medication, while clinicians are often uneasy or unwilling to offer options other than their preferred prescriptions.
A study from Mayo Clinic shows that a simple series of conversation cards can dramatically improve both the patient’s and their physician’s satisfaction with the discussion on and comfort with the choice of antidepressant. The findings appear in the journal JAMA Internal Medicine.
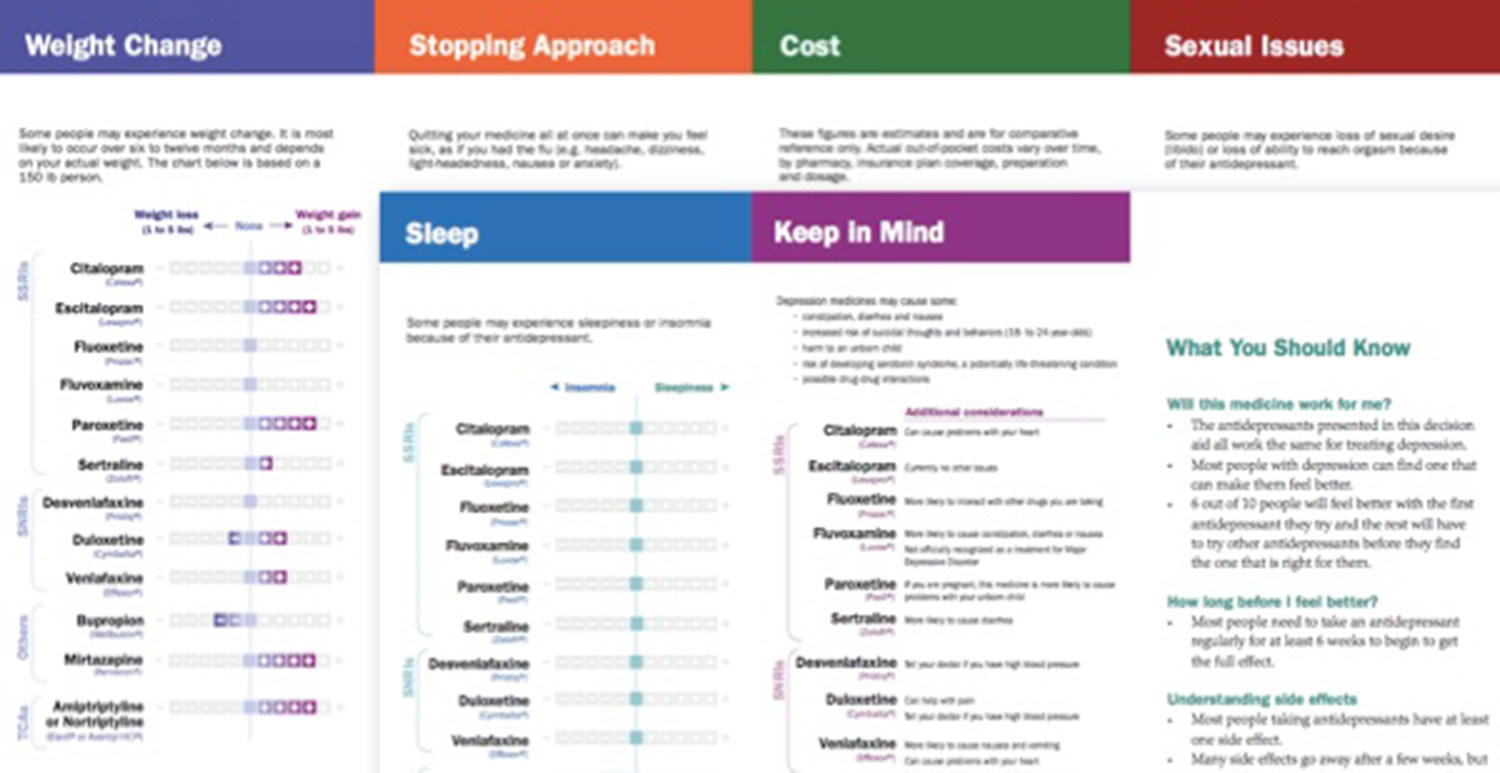
“We worked closely with patients, their families, and clinicians to fully understand what really matters to them when confronted with this situation. We wanted to transform the too-often unavailable evidence into accurate, easily accessible information to be used within the context of each person’s needs and preferences, ultimately creating what we hope to be meaningful conversations,” says Annie LeBlanc, first author and Mayo Clinic health science researcher.
This study evaluated information from 117 physicians and 301 patients from a range of Minnesota and Wisconsin communities. Compared to their usual care, patients said the use of decision aids improved their comfort in making decisions by 5 out of 100 points, their knowledge by 10 out of 100 points, and the likelihood of being satisfied by 2.4-fold, the study found. Physicians also reported an increase in decision-making comfort by 11 out of 100 points, a 1.6-fold increase in the likelihood of being satisfied. The extent to which they involve patients in the decision-making process during the clinical encounters increased by 16 out of 100 points. Interestingly, the use of the tool did not add to the length of the discussion.