A year and a half ago, Tiffany Aplet was a frequent visitor to the hospital emergency room.
She would go to the ER with shortness of breath and tightness in her chest, get admitted to the hospital, get her symptoms controlled and then get discharged.
About three weeks later, the cycle would repeat.
After the first visit to the ER, Aplet was diagnosed with chronic obstructive pulmonary disease, or COPD. She tried various medications prescribed by her primary care physician, but none of them seemed to fully relieve her symptoms.
Inevitably, her symptoms would spiral out of control — a COPD exacerbation — landing her in the hospital and causing her to miss a growing number of days at work.
“I was pretty sick,” said Aplet, now 58.
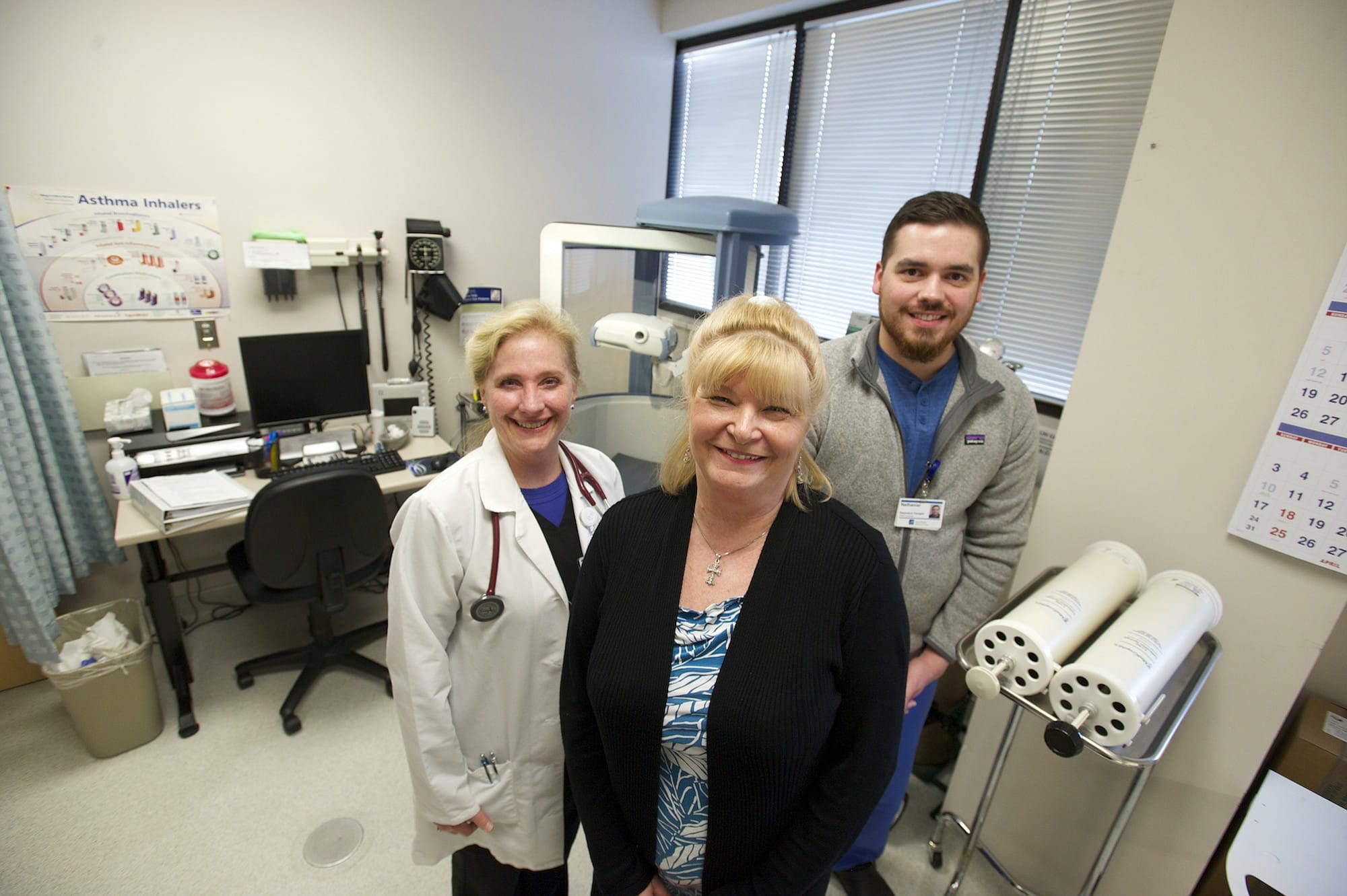
About a year ago, Aplet was referred to Rita Williams, a nurse practitioner at PeaceHealth Medical Group Pulmonary. That was about the same time the Vancouver medical group was beginning to craft a new program devoted to improving care for COPD patients and reducing hospital readmission rates.
COPD refers to a group of lung diseases that block airflow and make breathing difficult. Emphysema and chronic bronchitis are the two most common conditions that make up COPD, according to the Mayo Clinic.
COPD cannot be cured, and the damage to the lungs cannot be reversed. But treatment can help to control the symptoms and prevent additional damage to the lungs.
Symptoms of COPD include chronic cough, shortness of breath (especially during physical activity), wheezing, chest tightness, excess mucus in the lungs and frequent respiratory infections. People with COPD are also likely to experience exacerbations, when symptoms are more severe and last for several days.
The goal of the PeaceHealth COPD program is to prevent the exacerbations that lead to hospitalizations, Williams said.
“Every exacerbation that leads to hospitalization, because it was so severe, means lost lung function,” she said. “It speeds that decline of lung function.”
Last summer, prior to the program’s Aug. 1 launch, 25 of 100 patients with COPD were admitted to the hospital within 30 days of their previous discharge. In the months that followed, readmissions dropped to single digits, between one and three readmissions. So far this year, the hospital has had no 30-day COPD readmissions, even though the first quarter of the year has historically posted some of the highest admission numbers, according to PeaceHealth Southwest data.
Encouraging follow-ups
The program coordinates an array of services for patients who have been admitted to the hospital for COPD complications. Even patients who have not been admitted but have received a COPD diagnosis are set up with the program.
When a person diagnosed with COPD, or suspected to have COPD, is hospitalized, they are now immediately referred to PeaceHealth Medical Group Pulmonary for a follow-up appointment with a pulmonology provider upon discharge.
Many patients in the past were not established with a pulmonary clinic and were instead encouraged to follow-up with their primary care provider. It was up to the patient to make that appointment. Now, however, the clinic is notified when a COPD patient is referred for care.
“The goal is to get the patient in to see us within seven — no more than 10 — days after their hospital discharge,” Williams said.
Within 48 hours of hospital discharge, the patient also receives an at-home visit from a respiratory therapist, who follows up for 30 days post-hospitalization.
Once patients are part of the COPD program, they work with their pulmonary provider to establish an action plan that outlines responses to various changes in symptoms. The plan also identifies when a patient should take action to control symptoms — such as taking medication or monitoring peak flows — and when the patient needs to call 911.
Patients in the program also receive an annual pulmonary function test; education on the different types of inhalers and when each should be used; smoking cessation guidance; screening for related issues, such as sleep apnea, allergies and low oxygen levels; and referral to pulmonary rehabilitation, for those who qualify. The program staff also ensure patients are up to date on their flu and pneumonia vaccinations, as those illnesses most frequently cause complications that lead to hospital admission.
“The COPD clinic has helped us really focus on the things that are important to our patients,” Williams said.
Prior to launching the program, the providers were doing many of the same things. The program, however, has helped to organize the efforts, as well as get patients referred to the specialists sooner, Williams said.
Aplet was diagnosed with COPD in December 2013. She spent about five months working with her primary care provider trying to manage the disease before she was referred to Williams for specialty care.
Through the program Aplet received valuable education about her medications — the importance of taking them regularly, even when symptoms are controlled — and the aggravators that caused her COPD symptoms to flare.
Aplet also received help to quit smoking. A smoker since her teen years, Aplet hasn’t smoked in nine months.
“It’s been really good for me to come here,” Aplet said of the clinic. “I have my good days and my bad days, but I have a lot more good days than I did before.”