You’ve probably heard the stories before.
Maybe for football. Maybe for another sport. An athlete sustains a blow to the head. They’re told to shake it off and return to play. After all, they only got their bell rung. Had their clock cleaned.
Those stories are becoming less commonplace as concussion awareness rises, and the seriousness in concern around head trauma increases with that awareness.
While coaches and athletes change the way they view concussions, PeaceHealth Southwest Medical Center will also change the way it treats and rehabilitates sports-related concussions when the hospital’s new sports concussion rehabilitation program debuts Aug. 27. The program will be the first of its kind in Clark County.
“This program is going to help zero in on the sports-related aspect of concussions,” said Morgan Gilpin-King, an occupational therapist with the concussion rehab team. “The outpatient neuroclinic here at PeaceHealth does already treat concussions, but with a variety of diagnoses, ages, conditions or mechanisms of injury.”
Studies: Concussions common
The Centers for Disease Control and Prevention estimates that between 1.6 million and 3.8 million sports-related concussive injuries occur annually in the United States.
A 2017 CDC study drawing from almost 800 high school athletes found that 69 percent of them played with concussion symptoms, and 40 percent of them said their coach was not aware they had a possible concussion.
In matched sports in high school, girls were 12.1 percent more likely to sustain a concussion than boys, according to a 2017 study by the American Academy of Orthopaedic Surgeons.
A Journal of Athletic Training study found that concussions make up 8.9 percent of all high school athletic injuries and 5.8 percent of all college injuries.
The same study found that football (40.5 percent) had the highest rate of concussion, followed by girls soccer (21.5), boys soccer (15.4) and girls basketball (9.5).
Multiple disciplines
Since the program will focus specifically on sport concussions and include doctors working across multiple avenues of therapy, it should be more efficient in rehabbing athletes’ head traumas, officials said.
“We’ll be able to treat these patients quicker, and hopefully with higher frequencies, as well as have all the disciplines in one place,” said Melissa Bohnstedt, a speech language pathologist with the team.
The program will generally treat athletes ranging from middle school through college students, but it can also help your dad if he sustains a concussion taking a softball off the head at the company game.
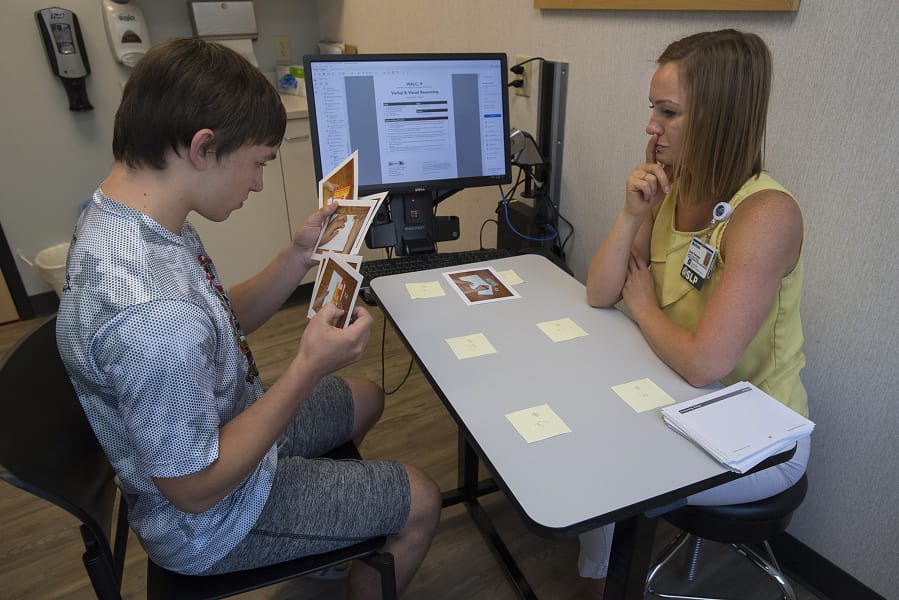
Depending on what’s needed, a patient could work with multiple therapists. Bohnstedt will work with patients on the cognitive side of the program. She will help them restore their ability to focus on tasks and rapidly switch attention between tasks. Her purview will also include problem solving and reasoning as well as memory.
“It’s not just a return to sports, although that’s our primary focus,” Bohnstedt said. “We want to make sure they’re successful returning to work, returning to their academic life, and make sure they’re successful and a well-rounded person.”
Gilpin-King will work with patients on visual and sensory processing changes.
“These kids might seem more moody or more irritable,” Gilpin-King said. “Or they get overstimulated a little more than normal, and so we address some strategies to help them kind of reintegrate their senses and tolerate all of their daily activities.”
Chris Garcia, a physical therapist and clinical specialist, will assist patients with neck injuries or vestibular dysfunction, and he will also make sure patients increase their exercise load in the proper manner while returning to activities.
“When you have a concussion, there’s a significant amount of cellular changes within the brain, and the brain doesn’t tolerate the exertion of exercise as well,” Garcia said. “You have to progressively increase the patients workload through exercise to not only help them back to their sport, but to help them recover quicker than they would if they were instructed to take it easy until their symptoms subside.”
Kelsy Parker, who works in physical medicine and rehabilitation with a focus on sports medicine, will assist “if things are more complicated: if they have headaches that are very limiting and they might need to start a medication, or if the symptoms are prolonged causing depression or other things where they might need a better level of involvement.”
The program’s August start is meant to coincide with school returning. For student-athletes in the program, a doctor from the concussion team will act as a point-person for that athlete. That point of contact person can be in touch with the athlete’s athletic trainer, and give updates on behalf of the entire concussion team, streamlining the process.
“I think the model is a fantastic idea,” Parker said. “Most health care places should go to it because if you have a multidisciplinary approach it eliminates a lot of wasted time. If we’re all in the same location, if there’s a cognitive concern, but there’s also neck pain and other things, then you can just go across the way and talk with whoever is treating the patient.”