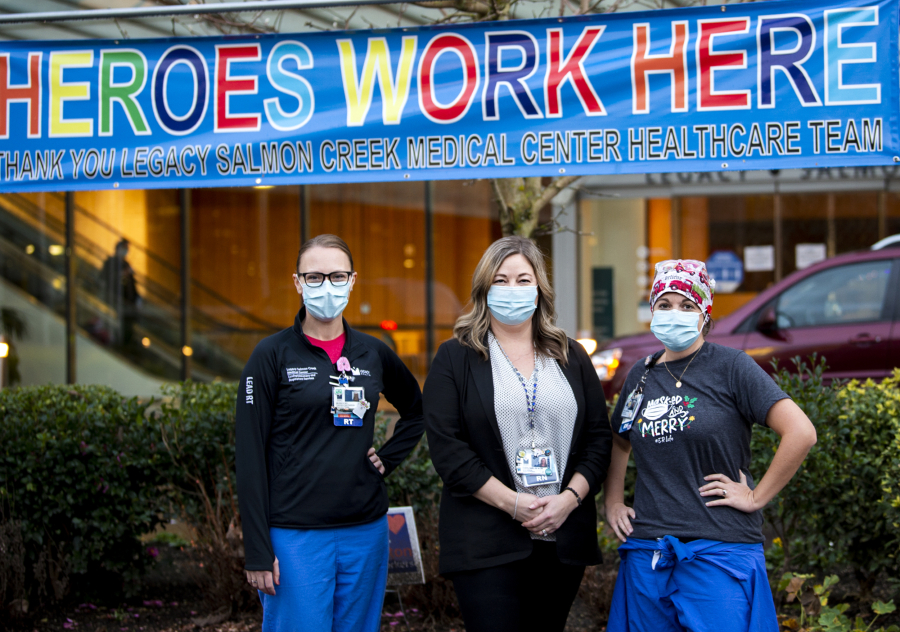
It’s hard for staff at Legacy Salmon Creek Medical Center not to run through worst-case scenarios when a new COVID-19 patient leaves their loved ones behind and checks into the hospital.
“You watch them say goodbye and you know in your head they might go to the ICU, get intubated and be dead tomorrow,” said Melissa Glascock, a lead respiratory therapist.