Do you know if your breasts are fatty or dense?
You should. If they’re dense, a Washington law that took effect in 2019 requires the letter reporting your mammogram results to include this paragraph:
Your mammogram indicates that you may have dense breast tissue. Roughly half of all women have dense breast tissue which is normal. Dense breast tissue may make it more difficult to evaluate your mammogram. We are sharing this information with you and your health care provider to help raise your awareness of breast density. We encourage you to talk with your health care provider about this and other breast cancer risk factors. Together, you can decide which screening options are right for you.
So what the heck does that mean?
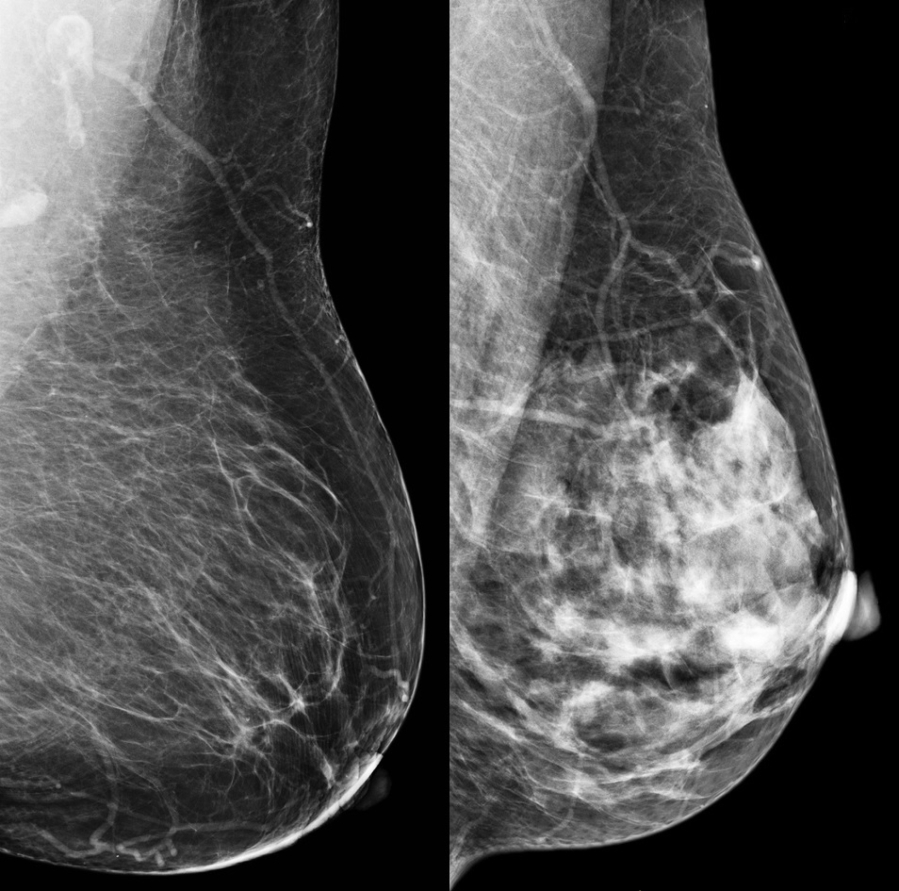
Breasts contain three types of tissue: glandular, fibrous and fatty. Breasts with less fatty tissue (which shows up dark on a mammogram) than glandular and fibrous tissue (which both show up white) are considered dense.
“The problem is cancer is also white on the mammogram,” said Dr. Jennifer Ochsner, a radiologist for Vancouver Clinic’s Breast Care Center. “That’s why we’re interested. The mammogram is harder to read.”