SEATTLE — From inside festival booths across the country, William Perry and Ingela Travers-Hayward hope to equip “an army of lifesavers.”
The pair co-founded This Must Be The Place, an Ohio-based nonprofit that distributes free naloxone at music festivals and concerts across the country, including Seattle’s Capitol Hill Block Party and Day In Day Out. So far in 2023, they have distributed 16,755 doses of Narcan, the nasal spray version of the lifesaving, opioid overdose-reversal drug naloxone.
Drug overdoses are soaring across the country, with the U.S. Centers for Disease Control and Prevention reporting a record of almost 108,000 deaths in 2021, driven primarily by fentanyl. Locally, fentanyl overdoses killed 700 people in King County last year — up 83% from 2021 and 323% from 2020 — and 147 in Snohomish County.
Fentanyl is a synthetic opioid up to 50 times stronger than heroin and 100 times stronger than morphine, and it’s the leading cause of death for American adults under the age of 45. Two salt-sized grains of fentanyl, Public Health — Seattle & King County said, can be enough to cause an adult to overdose.
If you’re going to a music festival, concert or event where you think people may be using recreational drugs, here’s what experts say you should know about naloxone and fentanyl test strips.
What to know about naloxone and Narcan
Naloxone (including the nasal version Narcan) is the only medication on the market that is effective in reversing opioid-related overdoses, which can be caused by prescription pill, heroin and fentanyl use.
In March, the U.S. Food and Drug Administration approved selling Narcan without a prescription, making it the first opioid treatment drug sold over the counter.
Perry said people have heard of Narcan, they’ve heard of naloxone, but an “overwhelming majority actually hasn’t seen this stuff in real life,” including nearly 80% of the people who receive a kit from their booth at events across the country.
By the end of this year, Perry and Travers-Hayward will have visited 27 major music festivals and over 60 events.
The duo anticipates they will distribute over 30,000 naloxone kits this year, aiming to fight the fentanyl epidemic by “normalizing naloxone and other overdose prevention tools in every corner of the country,” the nonprofit’s website says.
They focus on concerts and musical festivals because “the possibility of someone using a substance exponentially increases,” Perry said, especially among those who only use a few times a year.
When people visit the booth, Perry, who became a rehabilitation counselor after dealing with addiction and spending a decade in prison, often only has minutes to train people on how to use Narcan to save someone from an opioid overdose.
There are a lot of misconceptions about overdose reversal and overdose prevention, Perry said, shaped by “sensationalized things you might have seen in the movies,” like the dramatic “Pulp Fiction”-style anti-overdose injection to the heart.
But in reality, saving someone’s life is “really, really simple.” The nasal version of naloxone, which Perry said is the most user-friendly version, works just like Flonase.
“You shove it up somebody’s nose and squirt it,” Perry typically instructs people.
“It literally only does one thing,” Perry continued, which is binding to the opioid receptors in the body, kicking off the opioids and causing a person to breathe again.
Naloxone can take 30 seconds to a few minutes to bind to the brain receptors, reversing overdose symptoms such as slow breathing, tiny pupils and loss of consciousness.
Narcan is safe to use even if you are not sure someone needs it. It will not harm someone if they’re not suffering from an opioid overdose — “so, for example, if you’re misdiagnosing another medical situation,” Perry said — and there is no potential for abuse, according to the CDC.
Anyone of any age can acquire and administer naloxone under Washington state law. The state’s good Samaritan law also protects anyone who tries to help someone overdosing from facing civil liabilities and protects overdose victims from facing drug possession charges.
Naloxone can be found at many local pharmacies or community organizations, and it’s free if you have Medicaid. You can also order naloxone online for free using the Washington state order form or the King County order form.
Health professionals recommend people carry at least one dose on them, especially if a loved one is suffering from a substance use disorder or if they are around people at risk of an overdose.
What to know about fentanyl test strips
Although health officials say fentanyl test strips could help prevent accidental overdoses, they were illegal under Washington law until recently, once falling under the definition of drug paraphernalia.
House Bill 5536 went into effect July 1, raising the penalty for drug possession to a gross misdemeanor and clarifying that drug test kits are legal in Washington.
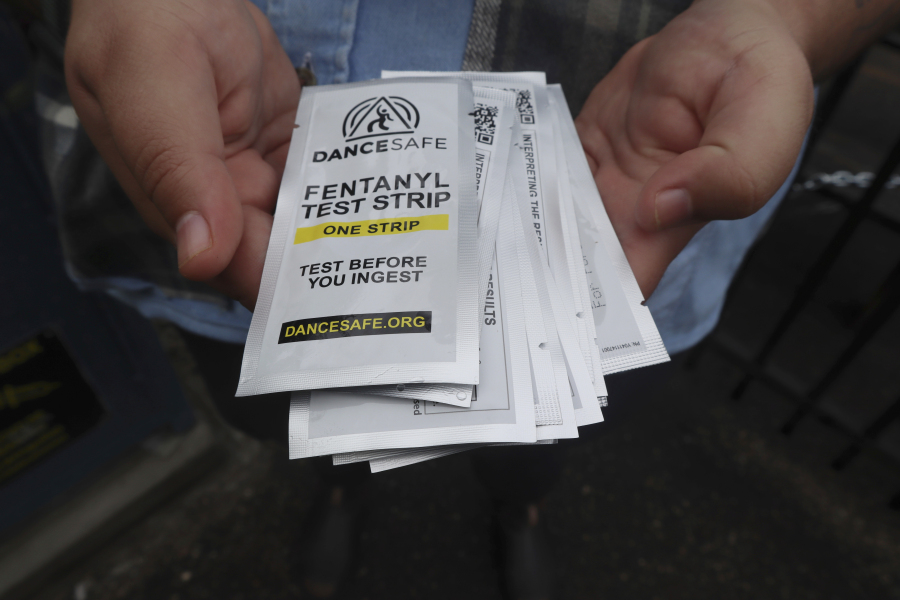
Strip testing, also known as immunoassay testing, involves diluting drugs in a certain amount of water and dipping a test strip into the mixture, according to DanceSafe, a nonprofit test kit manufacturer.
Test strips can’t tell you exactly what’s in a drug (only a lab can do that), but they can tell you whether one specific type of drug is present in a sample at all, providing a positive or negative result.
Each kind of test strip is specialized to detect a particular set of drugs. Fentanyl strips, for example, are only supposed to detect fentanyl and some of its analogs (drugs that are slight variations on fentanyl) in all different kinds of drugs (like cocaine, methamphetamine and heroin) and drug forms (pills, powder and injectables), according to DanceSafe and the CDC.
King County sends test strips to hospitals, colleges and universities, municipal courthouses, homelessness service providers, community groups and service organizations like Peer Seattle for distribution.
As part of a yearlong pilot program, two vending machines dispense the tests for free at Peer Kent and Peer Seattle, organizations that support addiction as well as behavioral and chronic health conditions.
The county will also mail test strips for free to anyone in King County, although it can take up to six weeks for delivery. Residents can request those online at redcap.iths.org/surveys/?s=ALWN9T3A3XY4MDMW.
Some businesses in Seattle also offer test strips for free, like Uncle Ike’s Pot Shop.
Lowering the risk of overdose
If you are going to an event soon, make sure to check with the venue or event organizers what overdose prevention tools are provided or allowed.
If you don’t use drugs, but are around people who do, “the best thing you can possibly do is just watch over people and take care of them,” Perry said.
“One decision shouldn’t be a death.”
Consider these tips from Perry and the CDC to keep yourself and others safe:
- Keep naloxone readily available on you and at home. Check with your local health department or community-based organization to see if they distribute naloxone at no cost. You can also talk with your health care provider or pharmacist about being prescribed naloxone (Narcan) if you or someone you know is at risk for an overdose.
- Avoid mixing drugs. Mixing multiple stimulants like methamphetamine and cocaine, depressants like opioids and alcohol or a combination of both can be deadly. “Go slow,” Perry said, “because you don’t have to do everything all at once.”
- Don’t rely on a previous source or experience. Knowing where your drugs come from doesn’t mean they’re safe. Even if you have used drugs before, your body could react differently every time.
- Never use drugs alone. Make sure the people around you are aware when you have taken drugs in case they need to give you naloxone or call for emergency assistance. Always let people know you have naloxone on hand and where you keep it in case of emergency. Three out of five overdoses happen either in a public place or with someone else, Perry said. That means 60% of these deaths are avoidable, he said.
- Don’t sleep it off. The worst advice someone can give to others or take themselves, Perry said, is to “just sleep it off … When people do go to sleep, unfortunately, with fentanyl, they oftentimes don’t wake up.”
- Ask for help if you’re ready to get treatment for your addiction. Recovery is possible — it’s OK to ask for help. You can find evidence-based treatment and service options near you by visiting findtreatment.gov or by calling 800-662-4357 any time.