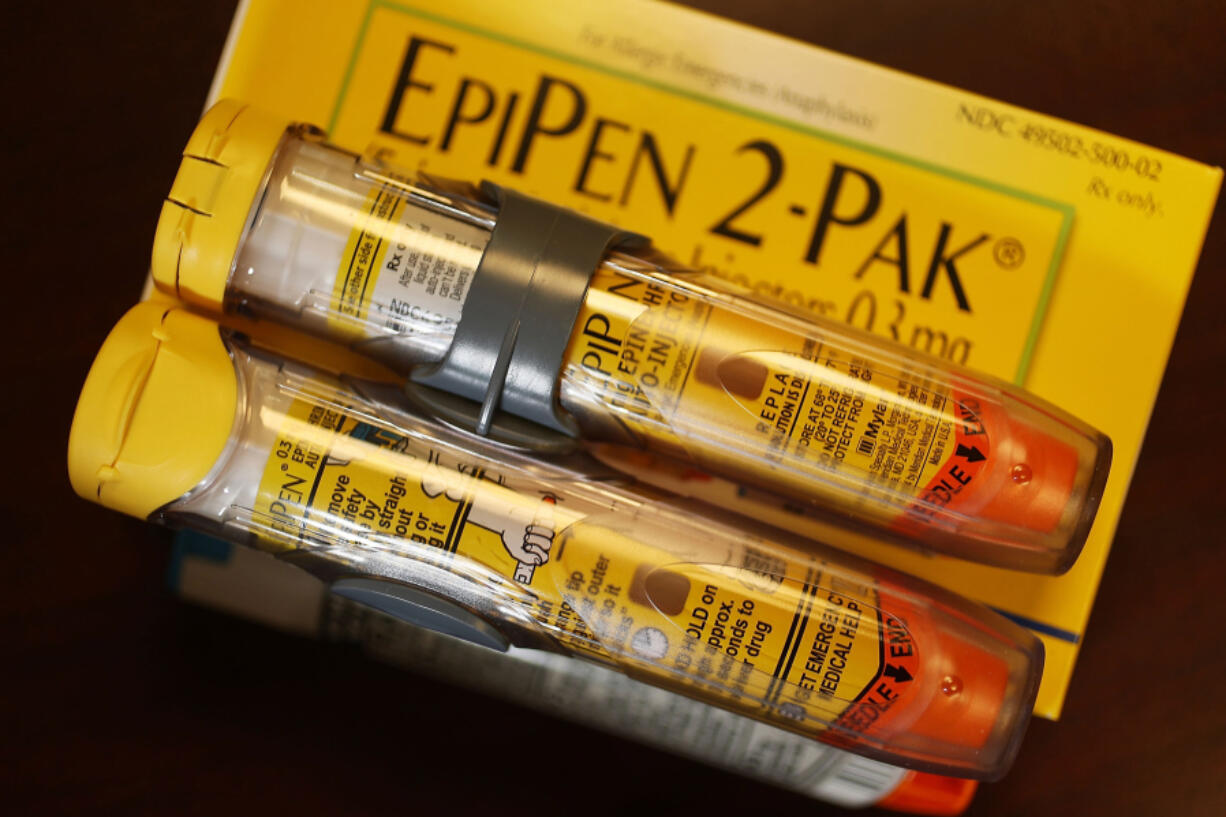
Laura Pleasants doesn’t leave her house without at least six EpiPens — autoinjectors about the size and shape of a whiteboard marker that contain medication that can calm a body’s allergic reaction.
She carries two in her laptop bag and another two in her purse. She’s taught all of her friends how to use one in case she’s experiencing a reaction so severe that she can’t do it herself.
Despite her caution, Pleasants — who has alpha-gal syndrome, an allergy to mammal meat caused by a bite from the lone star tick — estimates that since she was diagnosed in 2010, she’s experienced anaphylaxis about a dozen times. That’s a serious, potentially life-threatening, allergic reaction that can involve swelling in the throat, lips and tongue, shortness of breath, chest tightness and other symptoms.
So when Pleasants heard that the U.S. Food and Drug Administration had approved a medication to help people with food allergies avoid severe reactions, she was thrilled.
“It would change my life drastically,” said Pleasants, 52, who lives on Kent Island, Md., and works for an allergist in Bel Air. She added with a laugh, “All of my friends would actually want to go out to eat with me again.”
The FDA approved the medication omalizumab — co-developed by Novartis Pharmaceuticals and Genetech, and sold under the brand name Xolair — for use by some people with food allergies earlier last month.
While Xolair is the first FDA-approved medication for food allergies, it is not a cure. Someone with a peanut or wheat allergy, for instance, can’t start eating peanut butter and jelly sandwiches for lunch, even if they’ve been prescribed the drug. Instead, Xolair is meant to reduce the risk of allergic reactions that people may experience after accidental exposure to a food they’re allergic to.
It’s administered through regular injections every two to four weeks, with a frequency depending on a patient’s reaction to allergens and their weight. That’s a commitment, Pleasants acknowledged, but she’s still excited to try the drug.
“You also have to keep in mind that if you go to a restaurant and my chicken was cooked with your steak, then I’m not immediately going to die,” she said. “It’s going to give me a little extra layer of protection.”
The FDA approved Xolair to treat asthma in 2003, and later approved the drug to treat chronic hives and nasal polyps. Researchers have long suspected that it also might benefit people with food allergies, but the federal agency didn’t give doctors the green light to prescribe it until the recent completion of a study led by the Johns Hopkins Children’s Center.
In that study, scientists found that Xolair substantially reduced potentially life-threatening reactions in patients with peanut allergy and other common food allergies. After about 16 weeks, nearly 67 percent of the study participants treated with Xolair were able to tolerate 600 mg of peanut protein — an amount equal to about 2.5 peanuts — compared with 6.8 percent of participants who received the placebo.
Most participants treated with Xolair were able to tolerate even more peanut protein than 600 mg, the initial endpoint of the study. A majority could tolerate 4,000 mg of the protein, equivalent to about 15 peanuts, and nearly half were able to eat 6,044 mg of the protein, equal to about 25 peanuts.
Researchers in the study also found that Xolair significantly increased the amount of other allergens participants could tolerate, including tree nuts, milk, eggs and wheat. However, there was variability among participants; 14 percent of people treated with the drug could not even tolerate 30 mg of peanut protein.
Dr. Robert Wood, director of the division of allergy, immunology and rheumatology at the Hopkins Children’s Center and the study’s principal investigator, presented the data Sunday at the annual meeting of the American Academy of Allergy, Asthma and Immunology in Washington, D.C. The study’s findings also were published Feb. 25 in The New England Journal of Medicine.
Wood, who identified the study as one of the most important done on food allergies during his 40-year career, said his team will continue to study the drug’s potential. That includes how it compares with Palforzia, an oral immunotherapy product approved to help mitigate allergic reactions in patients between 4 and 17 years old who are allergic to peanuts.
“We don’t expect the FDA is ever going to approve a label saying, ‘You can start eating the food,’ ” Wood said, “but there will be practice guidelines and things that are developed to talk about how the drug might be used differently in one patient to another.”
Increase in allergies
Between 6 percent and 8 percent of children and 2 percent and 4 percent of adults have a food allergy in the U.S. — percentages that have grown in the past few decades for reasons researchers don’t entirely understand.
People with food allergies produce a type of allergen-specific antibody called immunoglobulin E. When they eat, touch or inhale the food they’re allergic to, the allergen binds to those IgE antibodies attached to their immune cells, which in turn signals those cells to release huge amounts of chemicals, including one called histamine. This is what causes allergic reactions.
Xolair acts as an anti-IgE drug, which means it binds to the antibody and stops it from binding to immune cells. While it has some limitations — the effects wear off if patients don’t get regular injections, for instance — allergist Dr. Manav Singla predicts it will be greatly beneficial to the quality of life for people with allergies.